Primary Bone Lymphoma of the Tibia: “The Chameleon Lesion of Bone” Mimicking Ewing Sarcoma on MRI
Introduction
Primary bone lymphoma (PBL) is a rare extranodal manifestation of non-Hodgkin lymphoma, accounting for less than 5% of all primary bone tumors. Its imaging characteristics often overlap with other aggressive bone neoplasms—most notably Ewing sarcoma—earning it the nickname “the chameleon lesion of bone.” Recognition of subtle radiologic features is critical for accurate diagnosis and timely treatment, especially in young adults presenting with diaphyseal lesions.
Case Presentation
A 23-year-old male presented with progressive pain and swelling around the right tibia. Physical examination revealed a firm, fixed, tender mass over the mid-diaphyseal region. Routine laboratory values were within normal limits. Direct radiography and MRI were performed to assess the nature and aggressiveness of the lesion.
Imaging Findings
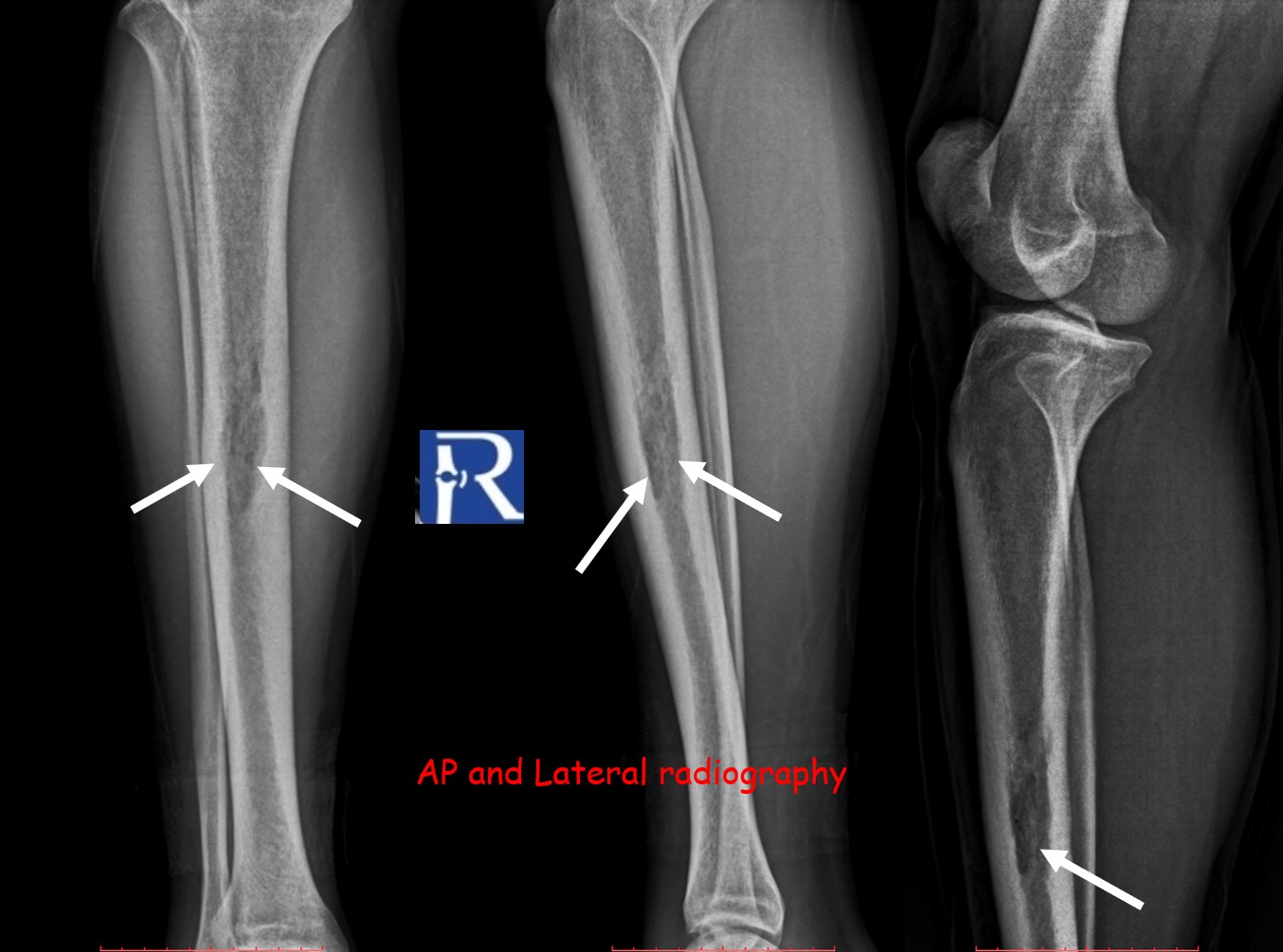
Plain radiography of the right tibia demonstrated a permeative lytic lesion at the mid-diaphysis, exhibiting aggressive characteristics but no periosteal reaction.
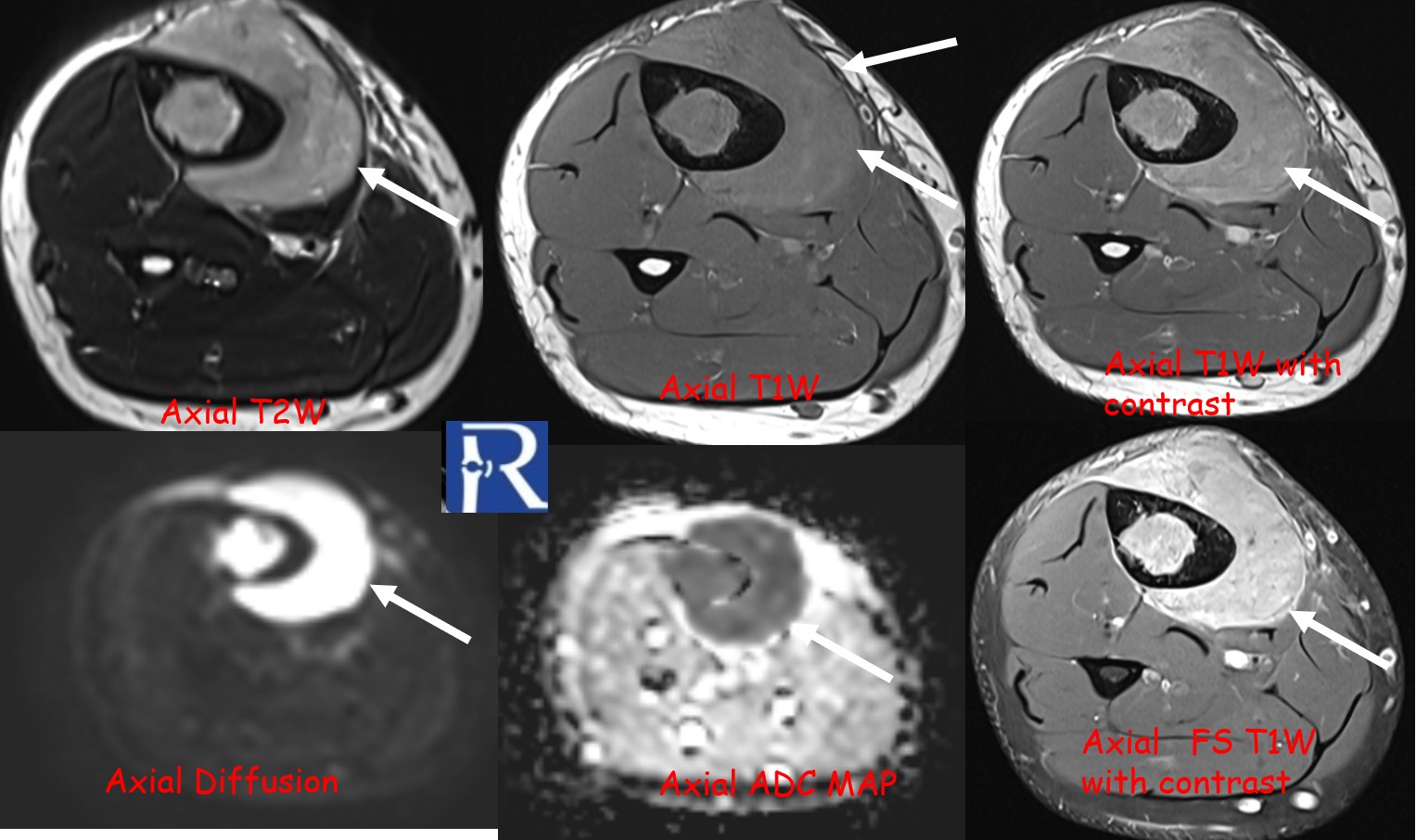
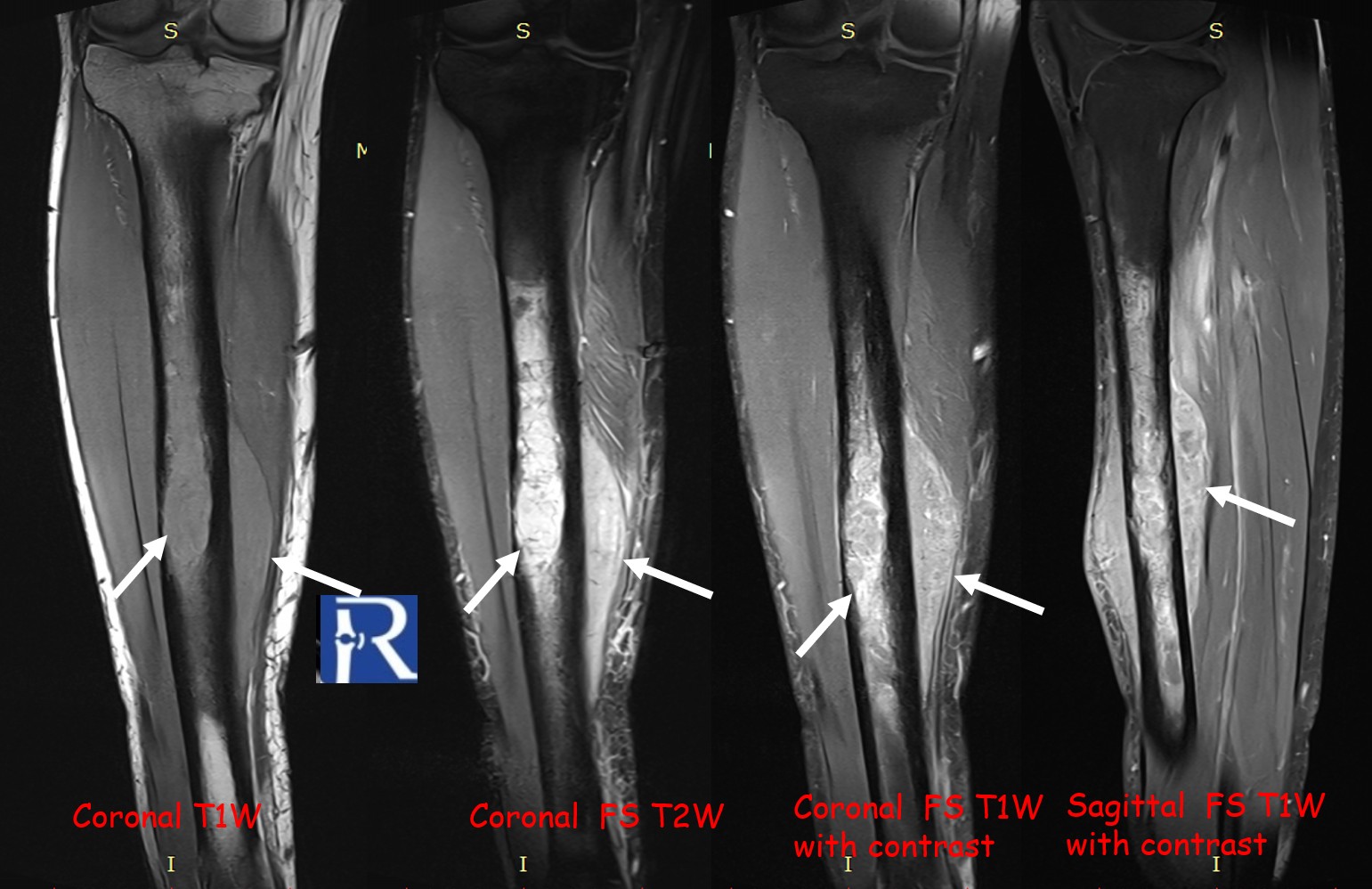
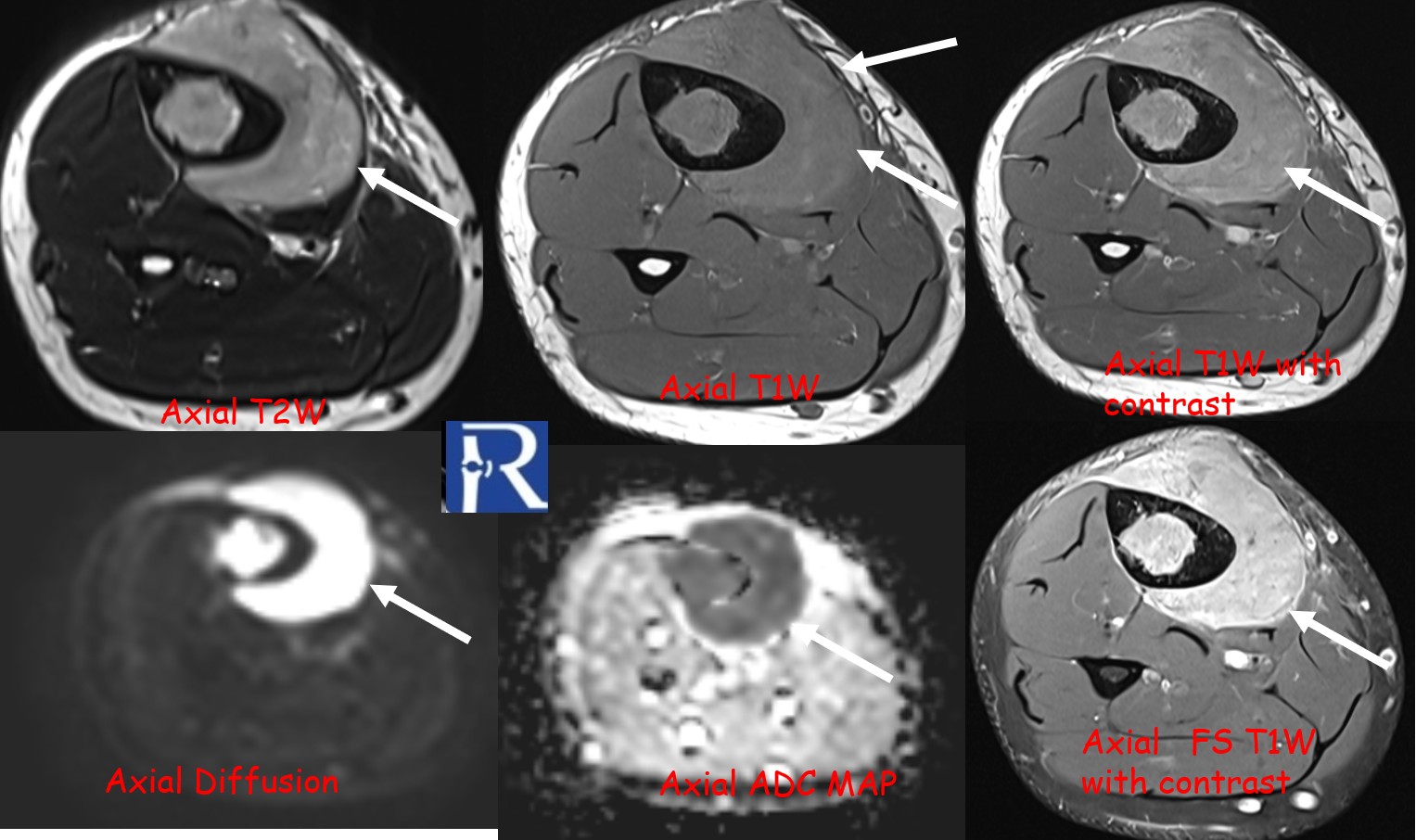
MRI revealed a significant soft-tissue component extending beyond the cortical margin, appearing hypointense on T1-weighted and intermediate on T2-weighted sequences, with heterogeneous contrast enhancement.
Diffusion-weighted imaging (DWI) showed marked diffusion restriction in both osseous and soft-tissue components, reflecting high cellularity.
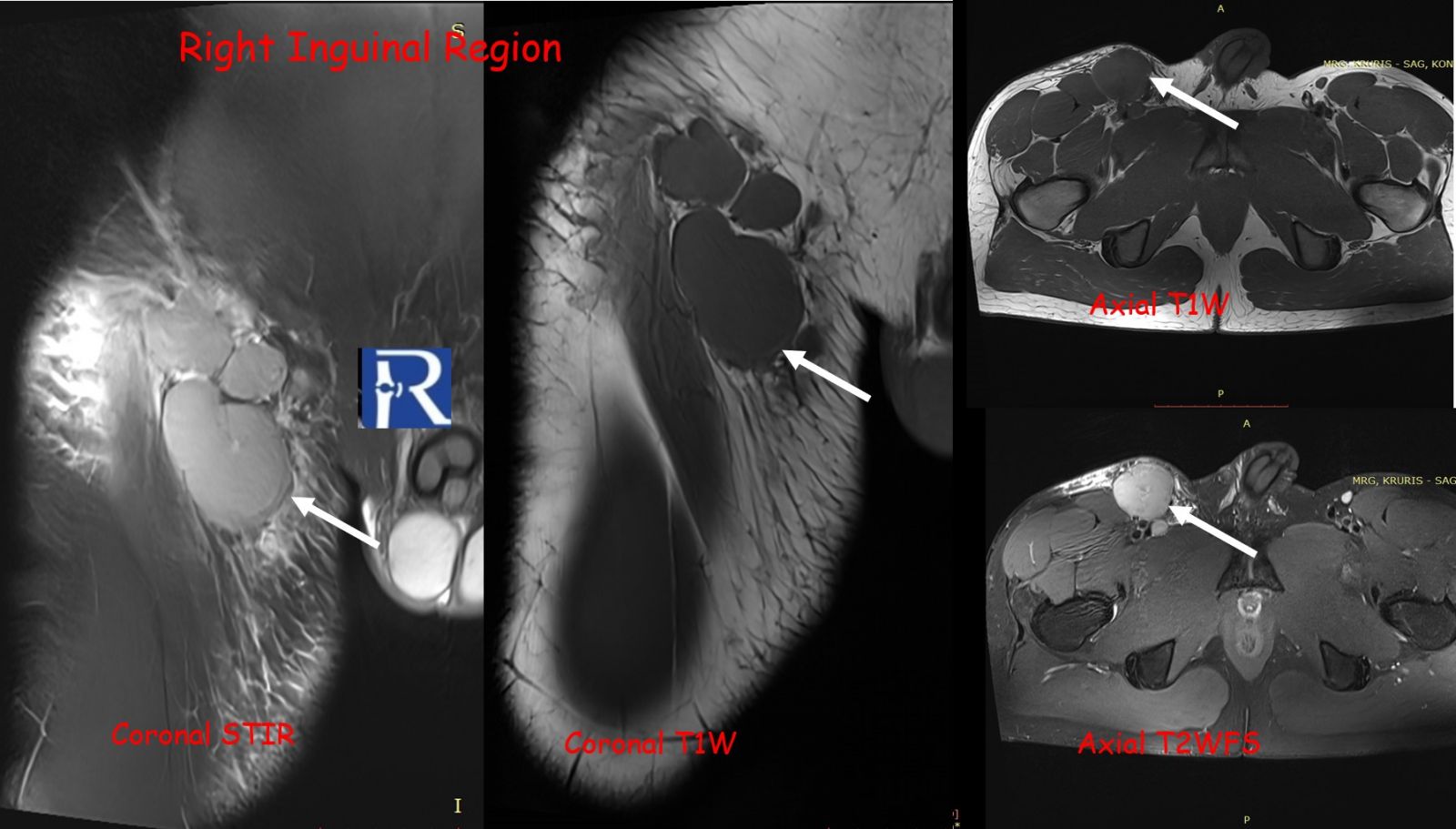
The lesion exhibited limited cortical destruction, yet extensive soft-tissue extension. Multiple conglomerate inguinal and pelvic lymph node enlargements were also identified, demonstrating signal characteristics similar to those of the primary lesion.
These imaging findings—particularly the absence of periosteal reaction, intermediate T2 signal, and marked DWI restriction—favored the diagnosis of lymphoma over Ewing sarcoma.
Histopathological analysis confirmed Diffuse Large B-Cell Lymphoma (DLBCL, Germinal Center B-cell type).
Immunohistochemistry: CD20+, CD45+, PAX5+, BCL6+, Ki-67 (98%), NKX2.2 negative, confirming a B-cell phenotype consistent with primary bone lymphoma.
Discussion
Primary bone lymphoma and Ewing sarcoma share overlapping radiologic characteristics, both often presenting as aggressive diaphyseal lesions with soft-tissue components. For this reason, they are collectively referred to as the “chameleon lesions of bone.”
However, certain imaging clues may guide the differential diagnosis. Lymphoma typically demonstrates limited cortical destruction, absence of periosteal reaction, and intermediate T2 signal intensity, whereas Ewing sarcoma tends to produce more prominent periosteal layering and higher T2 hyperintensity. Diffusion-weighted imaging is a powerful adjunct, with strong restriction patterns highly suggestive of lymphoma due to its dense cellular structure.
This case illustrates how radiologic–pathologic correlation is vital for differentiating PBL from small round blue cell tumors, such as Ewing sarcoma. Accurate diagnosis impacts management, as PBL responds well to combined immunochemotherapy (e.g., R-CHOP regimen) and radiation, whereas Ewing sarcoma typically requires surgical resection with adjuvant chemotherapy.
Conclusion
This case highlights the importance of recognizing primary bone lymphoma as a potential diagnosis in young adults presenting with diaphyseal aggressive bone lesions.
When encountering a permeative lytic lesion with extensive soft-tissue extension but limited cortical destruction and no periosteal reaction, lymphoma should be strongly considered.
Diffusion-weighted MRI plays a crucial role in differentiating lymphoma from Ewing sarcoma, reinforcing its value in musculoskeletal tumor imaging.


0 COMMENTS
These issues are no comments yet. Write the first comment...